Systemic lupus erythematosus (SLE), the most common form of lupus, is an autoimmune disease, which means that the immune system malfunctions and attacks the body’s own tissues. While some autoimmune diseases affect just one organ, in the case of lupus, many parts of the body can be affected.
As a result, symptoms vary widely and are often similar to other conditions, which need to be ruled out before a diagnosis can be made. Lupus therefore often goes undetected or misdiagnosed for long periods. Yet early diagnosis is important to manage the symptoms of lupus, initiate treatment to reduce the risk of long-term complications, and enable access to wider support (e.g. local patient groups).
It is estimated that 1.5 million Americans, and at least 5 million people worldwide, have a form of lupus, and that 90% of people living with lupus are women, with most developing the disease between the ages of 15 and 44. There is a higher prevalence of lupus among people of Asian and Afro-Caribbean origin than in Caucasians.
In SLE, the immune system malfunctions and attacks the body’s own tissues, which can affect the skin, joints, kidneys, heart, and other organs. As any part of the body can be affected by SLE, the condition can manifest itself in a multitude of ways.
There is no cure for SLE, and a significant need exists for safe and effective therapies. Most people with SLE are prescribed a combination of different medications to manage their symptoms, improve their quality of life, and reduce the risk of more serious complications.
The choice of treatment depends on how the patient with SLE presents – which part of their body is affected and the severity of the condition at the time.
The only approved treatments for SLE are acetylsalicylic acid (aspirin), hydroxychloroquine (an antimalarial), corticosteroids, belimumab, and anifrolumab. Some other immunosuppressive therapies are used off-label.
While the cause of SLE is not fully known, T and B lymphocytes are considered the key immune cells that play a role in the development of the disease. In individuals with SLE, both T and B cells become overactive. The main consequence of this increased activity is the infiltration of immune cells into different tissues and the production of autoantibodies, leading to inflammation and organ damage.
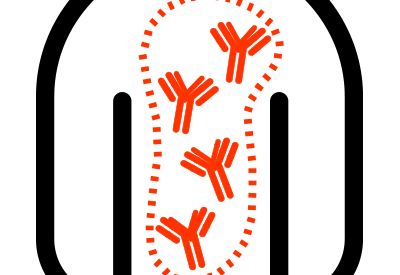
T and B lymphocytes have S1P1 receptors on the surface which enable the lymphocytes to detect the signaling molecule sphingosine-1-phosphate or S1P, which is responsible for lymphocyte trafficking from the lymph nodes to the blood. As an S1P1 receptor modulator, cenerimod inhibits the egress of T and B lymphocytes from lymph nodes. This prevents their migration and infiltration into the various organs, thus affecting the immune response that causes the multiple symptoms of lupus at a fundamental point in the cascade.
Based on the results of our Phase 2 studies, we now understand that cenerimod not only decreases the trafficking of T and B lymphocytes but also acts on the other key aspects of SLE. Indeed, cenerimod reduces the transport of autoantigens by professional antigen-presenting cells to the lymph nodes and, consequently, autoantigen presentation and lymphocyte activation. Further, cenerimod reduces pro-inflammatory cytokines and therefore inflammation. As a result, cenerimod will interrupt the vicious circle of SLE pathogenesis. Cenerimod is unique in tackling T cells, B cells, antigen-presenting cells, and inflammation, providing effective treatment for multiple aspects of lupus pathogenesis.

Cenerimod, the result of 20 years of research in Idorsia’s labs, is a highly selective S1P1 receptor modulator, given as an oral once-daily tablet. Cenerimod potentially offers a novel approach for the treatment of SLE, a disease with a significant impact on patients and limited treatment options. Cenerimod has been tested in several clinical studies, including a Phase 2a proof-of-concept study and the Phase 2b CARE study in patients with SLE, as well as a clinical pharmacology program.
As an S1P1 receptor modulator, cenerimod inhibits the egress of T and B lymphocytes from lymph nodes. This prevents their migration and infiltration into the various organs, thus affecting the immune response that causes the multiple symptoms of lupus at a fundamental point in the cascade. Based on the results of our Phase 2 studies, we now understand that cenerimod not only decreases the trafficking of T and B lymphocytes but also acts on the other key aspects of SLE. Indeed, cenerimod reduces the transport of autoantigens by professional antigen-presenting cells to the lymph nodes and, consequently, autoantigen presentation and lymphocyte activation. Further, cenerimod reduces pro-inflammatory cytokines and therefore inflammation. As a result, cenerimod will interrupt the vicious circle of SLE pathogenesis. Cenerimod is unique in tackling T cells, B cells, antigen-presenting cells, and inflammation, providing effective treatment for multiple aspects of lupus pathogenesis.
In November 2021, Idorsia announced the results of CARE, a double-blind Phase 2b study in which 427 adult patients with moderate to severe SLE on stable background therapy were evenly randomized to receive cenerimod (0.5, 1, 2, 4 mg) or placebo. The study duration was 18 months, with two 6-month treatment periods and a 6-month follow-up. After the first 6 months, patients on 0.5, 1, or 2 mg cenerimod and on placebo continued the same blinded treatment, while patients taking cenerimod 4 mg were re-randomized to blinded cenerimod 2 mg or placebo so as to permit assessment of the reversibility of lymphocyte reduction.
The primary endpoint was change from baseline to Month 6 in the modified (to exclude leukopenia) Systemic Lupus Erythematosus Disease Activity Index 2000 (mSLEDAI-2K) score. Secondary endpoints were improvements in the SLE Responder Index 4 (SRI-4) and the British Isles Lupus Assessment Group 2004 index (BILAG-2004). The study did not meet its primary endpoint after type I error control. However, the reduction in mSLEDAI-2K from baseline to Month 6 with cenerimod 4 mg versus placebo was nominally statistically significant: least squares (LS) mean difference -1.19 (p=0.0291). This effect was greater in patients with greater disease severity and patients with high type 1 interferon gene expression signature status.
The most frequent treatment-emergent adverse events reported with an incidence over 5% in any group and higher than placebo during six months of treatment were abdominal pain, headache, and lymphopenia. A reversible decrease in lymphocyte count is linked to the mechanism of action of cenerimod and, as expected, lymphopenia was seen more often in patients treated with the higher doses (2 mg and 4 mg). Importantly, there was no increased rate of infections compared to placebo: 0.5 mg: 23.5%; 1 mg: 11.8%; 2 mg: 19.8%; 4 mg: 20.2%; placebo: 18.6%. At Month 12, the incidence of adverse events reported was between 60% and 80% across all treatment groups, with no dose relationship: 0.5 mg: 63.1%; 1 mg: 81.2%; 2 mg: 77.0%; placebo: 70.9%. For patients in the 4 mg group re-randomized to either 2 mg cenerimod or placebo, the incidence of adverse events was 77.1% and 65.7% respectively. Compared to placebo, as seen during the first 6 months, treatment with cenerimod was not associated with an increased risk of infections.
These results provided the information needed to design a Phase 3 development program, including the patient population, optimal dose, and endpoints.
Current status
In December 2022, Idorsia initiated the OPUS program (Oral S1P1 Receptor ModUlation in SLE), which consists of two multicenter, randomized, double-blind, placebo-controlled, parallel-group Phase 3 studies to evaluate the efficacy, safety, and tolerability of cenerimod in adult patients with moderate to severe SLE on top of background therapy.
The main objectives of the program are to evaluate the effectiveness of cenerimod 4 mg in reducing disease activity, as well as controlling the disease, compared to placebo. The primary endpoint is change in the mSLEDAI-2K score from baseline to Month 12. Secondary endpoints include SRI-4 at Month 12 and – for the first time in a lupus registration study – measures of sustained disease control: time to first confirmed 4-month sustained mSLEDAI-2K response and time to first confirmed 4-month sustained response in mucocutaneous manifestations (i.e. rash, alopecia, mucosal ulcers).
The study design was informed by the Phase 2a study with cenerimod showing a dose-dependent reduction in plasma interferon-alpha, feedback from the lupus community, and data from the Phase 2b CARE study suggesting that the treatment effect of cenerimod was greater in patients with higher disease activity and persistent inflammation. The study includes eligibility criteria, and a screening period of up to 60 days, to ensure that only patients with true moderate to severe SLE are enrolled. Those who complete the 12-month double-blind treatment period will have the option to enroll in an open-label extension study, where all patients will receive cenerimod for at least one year.
The investigation of cenerimod for the treatment of SLE has been designated as a “fast-track” development program by the FDA. This designation is intended to promote communication and collaboration between the FDA and pharmaceutical companies for drugs that treat serious conditions and fill an unmet medical need. The Phase 3 program has been discussed with health authorities.
The Phase 3 program with cenerimod is currently recruiting patients, with a target enrollment of 840 adult patients with moderate to severe SLE from around 25 countries, including Japan.
Milestones
2022 Initiation of a Phase 3 program
2021 Phase 2b study provides clear pathway to Phase 3
2018 Initiation of a Phase 2b study
2015 Initiation of a Phase 2 safety study
Key scientific literature
- Hermann V, et al. Lupus Science & Medicine 2019;6:e000354. doi:10.1136/lupus-2019-000354
- Strasser DS, et al. RMD Open. 2020;6:e001261.
- Juif P-E,et al. Int. J. Mol. Sci. 2017, 18, 2636; doi:10.3390/ijms18122636
- Piali L, et al. Pharmacol Res Perspect. 2017 Dec;5(6).
- Borchers AT, et al. Autoimmun Rev. 2010; 9(5):A277-87.
- Pons-Estel GJ, et al. Semin Arthritis Rheum. 2010; 39(4):257-68.
- Govoni M, et al. Lupus. 2006; 15:110-113.
- Rahman A, Isenberg DA. N Engl J Med. 2008; 358:929-39.
- Abu-Shakra M, et al. J Rheumatol 1995; 22(7):1259-64.